Mariana Loureiro, MS4, Laura Mercer MD, MPH, MBA
Importance: Cesarean deliveries are common in the United States, with the majority considered to be nonelective cesarean deliveries occurring during labor, after membrane rupture, or for maternal or fetal emergencies. Traditionally, given the risk of surgical site infection, the pre-incision prophylaxis of choice had been a cephalosporin for both elective and nonelective cesarean deliveries. In 2016, Tita et. al. published a study supporting the use of adjunctive azithromycin to further reduce the incidence of postpartum infections, leading to an official update in the ACOG recommendations.
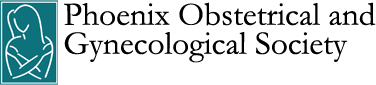
Objective: To determine to what degree teaching and non-teaching hospitals in a single hospital system in Arizona have effectively implemented the addition of adjunctive azithromycin prophylaxis in nonelective cesarean deliveries.
Design: Retrospective data of women who underwent nonelective cesarean deliveries in 2019 were collected from the electronic health record for both teaching and non-teaching hospitals.
Participants: Pregnant patients at Banner University Medical Center Phoenix (BUMCP), Banner Thunderbird Medical Center (BTMC), and Banner Ironwood Medical Center (BIMC) were identified by a positive history of unscheduled/labored cesarean deliveries, excluding allergy to azithromycin, non-singleton pregnancies, history of cardiac disease, presence of clinically diagnosed intraamniotic infection/chorioamnionitis, history of liver disease, a serum creatinine level of more than 2.0 mg per deciliter, and known substantial electrolyte abnormalities. These exclusion criteria are reflective of those in the index study.
Main outcomes: The primary outcome measured in this study was the number of pregnant patients in 2019 receiving adjunctive azithromycin prophylaxis prior to nonelective cesarean sections at a teaching hospital and two non-teaching hospitals. Secondary outcomes included time of azithromycin administration (before incision versus after incision/recovery), time of delivery (day of the week), gestational age at delivery, age of patient, race/ethnicity, patient’s home zip code and BMI.
Results: A total of 844 charts were reviewed for women who had undergone nonelective cesarean sections, with 149 nonelective cesarean sections at a teaching hospital (Banner University – Phoenix) and 112 at non-teaching hospitals (Banner Ironwood and Banner Thunderbird). Mean age and BMI were significantly different between the two types of hospitals. A mean age of 30.83 (SD 5.93) was found at the teaching hospital and a mean age of 28.93 (SD 6.04) at the non-teaching hospitals (P .0115). A mean BMI of 34.30 (SD 7.69) was found at the teaching hospital and a mean BMI of 36.99 (SD 12.86) at the non-teaching hospitals (P .0385). There were no significant differences between race or gestational age. Azithromycin was administered to 83 women (56.46%) at the teaching hospital and to 10 women (8.39%) at the non-teaching hospitals, with a significant difference among administration rates. Azithromycin was administered prior to delivery in 86.75% of cases at the teaching hospital and in 60% of cases at the non-teaching hospitals, with a significant difference in administration rates prior to delivery. The odds ratio of azithromycin being administered at a teaching hospital compared to a non-teaching hospital was 13.10 (95% CI, 6.33 – 27.10) without adjustment for age, BMI, race, and gestational age. When adjusted for these factors, the odds ratio was 18.67 (95% CI, 8.06 – 43.31). There was a significant difference in indication for azithromycin administration among both hospitals, with 11.11% of cases attributed to abruption or suspected abruption, 35.56% to arrest of fetal descent, 30.77% to cephalopelvic disproportion, 22.22% to failed TOLAC, 34.38% to fetal intolerance, 54.17% to lack of progressive cervical dilation, and no cases attributed to placenta previa. Azithromycin administration rates significantly differed among days of the week, with 34.62% administration on Monday, 43.18% on Tuesday, 21.88% on Wednesday, 20% on Thursday, 48.98% on Friday, 45.71% on Saturday, and 31.25% on Sunday.
Conclusions and Relevance: This study demonstrates that teaching hospitals were significantly more likely to administer adjunctive azithromycin compared to non-teaching hospitals, indicating a possible knowledge gap between academic and community centers. Despite this, azithromycin prophylaxis was only administered for 56.46% of nonelective cesarean sections at the teaching hospital. In cases in which azithromycin was administered, there were significant differences in timing of administration. The current guidelines indicate that azithromycin should be administered prior to delivery, and this was only evident in 86.75% of cases in the teaching hospital and 60% of cases in the non-teaching hospitals. Overall, the results highlight a gap in quality patient care. Both hospital types could benefit from implementing pre-operative order sets that include azithromycin administration, or a flagging system to remind providers that they are missing this medication as part of their orders. This could eliminate any uncertainty regarding when azithromycin administration is appropriate and establish the consistency needed to uphold quality patient care. The significantly lower azithromycin administration rate in non-teaching hospitals indicates the need for increased intervention within these hospital centers to keep up with their academic counterparts.
Michelle Goforth, MS3, Dean V. Coonrod, MD, MPH. Maureen Sutton, MPH, Maria Manriquez MD and Linda R Chambliss MD, MPH
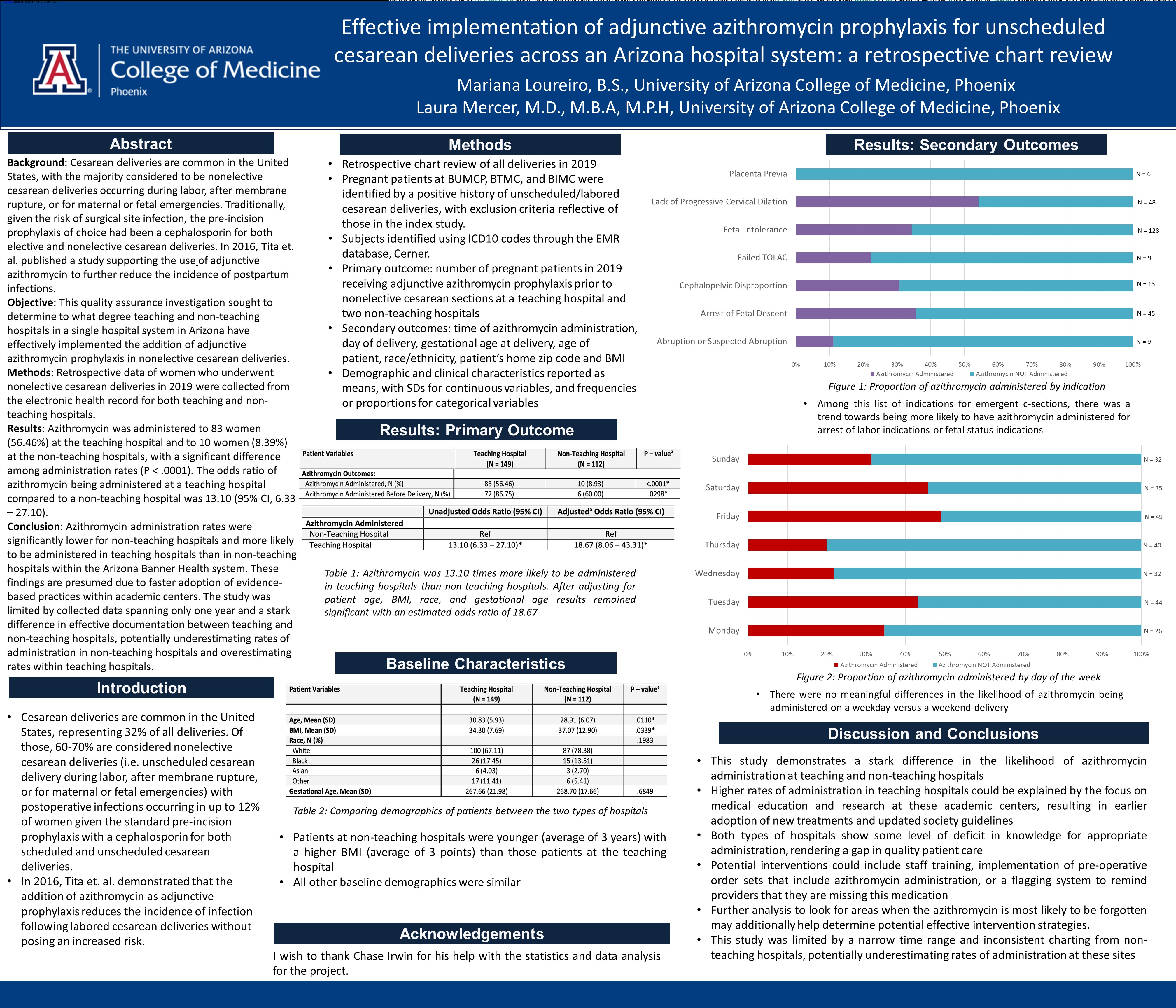
Introduction:Adverse childhood experiences (ACEs) have been shown to have lifelong consequences for health with higher incidence of several chronic diseases as well as substance abuse and adverse pregnancy outcomes. 1,2 High scores have been shown to predict chronic diseases regardless of socioeconomic status.1 Many women, especially with limited resources, only seek health care during pregnancy, making it an ideal time to assess the ACE score. We sought to determine the prevalence of high ACE scores in our patients and to determine if this is a risk factor for substance abuse before or during pregnancy.
Materials and Methods: Pregnant patients receiving care in a variety of clinic settings in our safety net hospital were approached and asked to complete a validated ACE questionnaire in English or Spanish. Interpreters were available for Spanish speakers as requested. A high score was defined as a score of > 4. 3
Results: 282 Adverse Childhood Experience (ACE) questionnaires were completed in a 9-month period in 2022 and early 2023: 251 questionnaires were completed in English and 30 in Spanish. The average score was 2.09 and 68 subjects (24.1%) had a score of greater than or equal to 4. 214 had low scores. Of those with high scores, 16 (23.5%) had a documented history of substance abuse. 6 patients reported abstinence during pregnancy while 10 admitted to on-going use. Of the 214 low-risk patients, 12 (5.6%) had a documented history of substance abuse and 6 admitted to on-going use during pregnancy. This is a relative risk of 4.2 (95% CI 5.2, 1.6) for having a history of substance use. We did not find that a high score predicted on going use in pregnancy.
Conclusion: Our patients were 50% more likely to report a high ACE score than the 16.7% reported U.S. prevalence. 3 High scores are associated with past or on going substance abuse in pregnancy. Not all patients had drug screens to confirm use or abstinence; this was by self-report and may be an underestimation. The ACE score during prenatal care, especially in safety net hospitals, is important in assessing risks in pregnancy, future health and substance abuse.
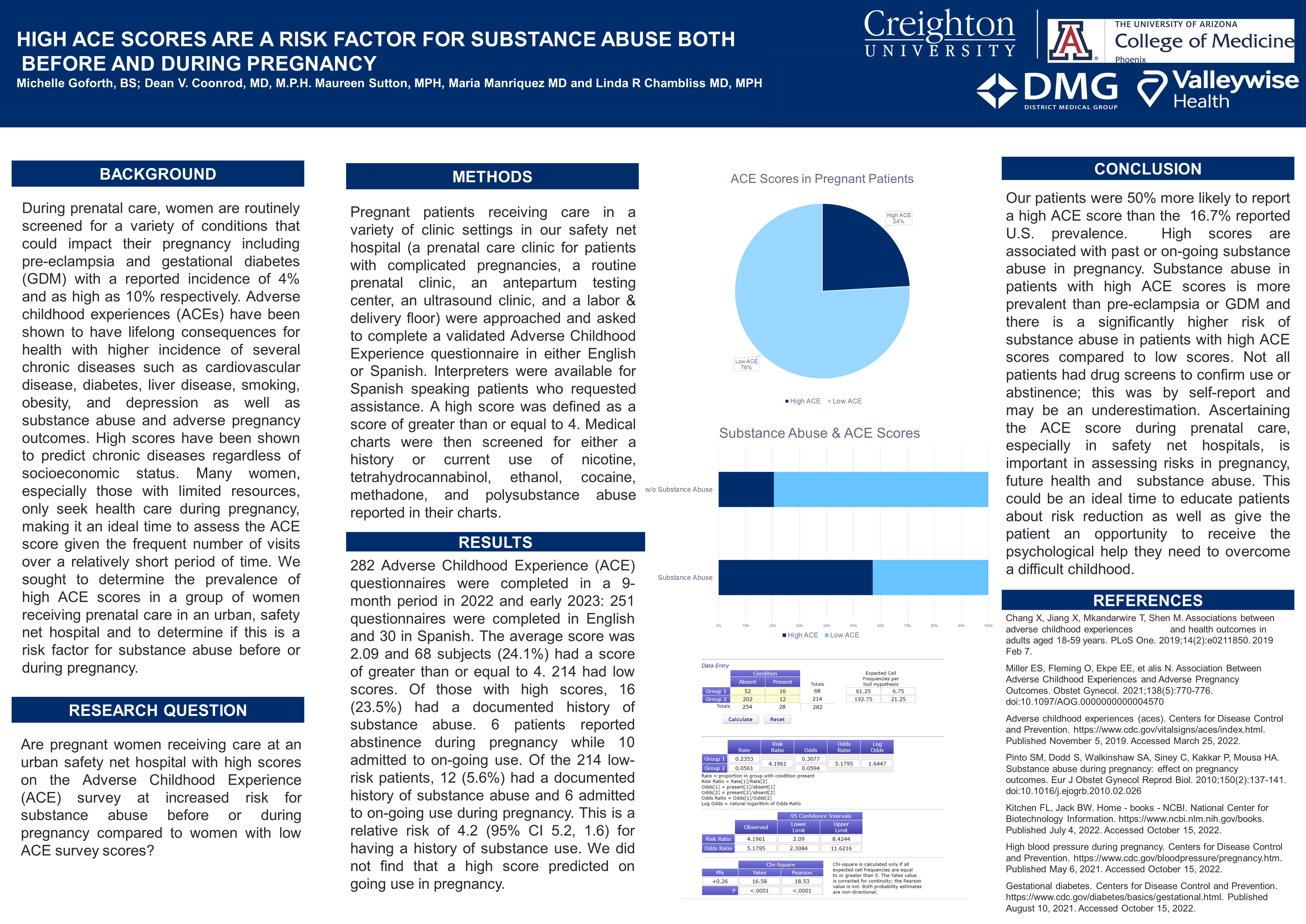
Mary Caitlin Indart, MD, Sheena Galhotra MD, Chengcheng Hu PhD, Katie Zeng MD, Gabriella Smith MD, Elizabeth Mangone MS4, Rachael Smith DO, Nichole Mahnert MD
OBJECTIVE: To compare surgical outcomes for laparoscopic hysterectomy between female and male gynecologic surgeons.
METHODS: This retrospective comparative cohort study was conducted at a single-site academic tertiary care medical center. Patients, age 18 years or older, who underwent laparoscopic (either conventional or robotic) hysterectomy for benign indications between January 2019 and December 2020 were included. Surgical outcomes were analyzed between the male and female surgeons.
RESULTS: A total of 560 laparoscopic hysterectomies were performed by 24 surgeons, which included 244 cases by 14 female surgeons and 316 cases by 10 male surgeons. Female surgeons performed significantly more conventional laparoscopic hysterectomies, while male surgeons performed more robotic hysterectomies. No statistically significant differences in the primary outcomes of hospital readmission rates, surgical complications, and postoperative complications were noted between the two groups. Also, no significant differences were noted in operative time, length of hospital stay, estimated blood loss, conversion to other surgical approach, emergency department visits in first 60 days, and 60-day mortality. Surgeon characteristics, such as sub-specialty training, surgical volume, years in practice, and practice setting were obtained and controlled for.
CONCLUSION: Female and male gynecologic surgeons have equivalent surgical outcomes, highlighting that they are equally capable of providing patients with high-quality surgical management.
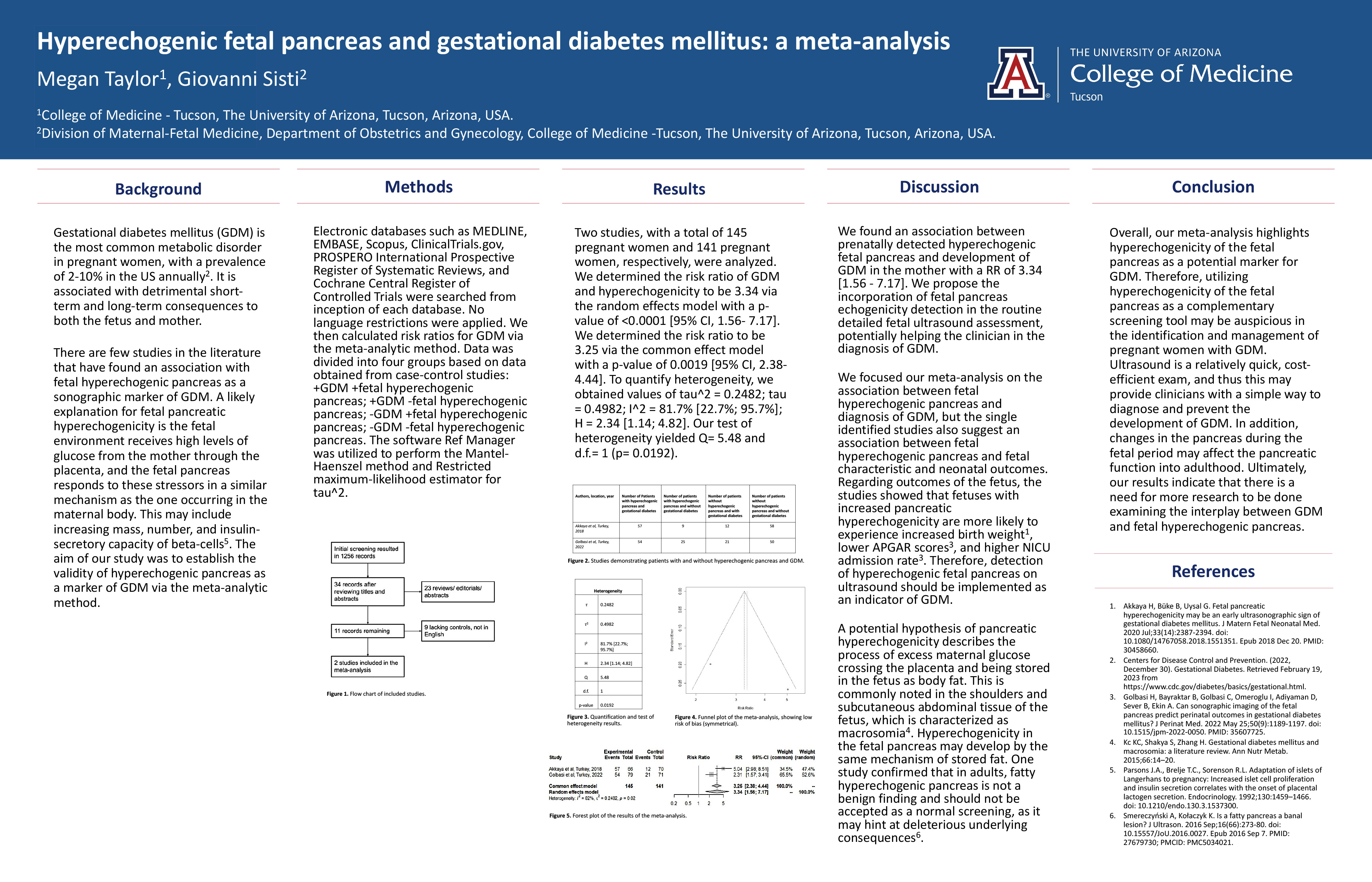
Megan Taylor, MS3, Giovanni Sisti, MD
Introduction: Gestational diabetes mellitus (GDM) is the most common metabolic disorder in pregnant women, with a prevalence of 2-10% in the US annually. It is associated with detrimental short-term and long-term consequences to both the fetus and mother. There are few studies in the literature that have found an association with fetal hyperechogenic pancreas as a sonographic marker of GDM. A likely explanation for fetal pancreatic hyperechogenicity is the fetal environment receives high levels of glucose from the mother through the placenta, and the fetal pancreas responds to these stressors in a similar mechanism as the one occurring in the maternal body. This may include increasing mass, number, and insulin-secretory capacity of beta-cells. The aim of our study was to establish the validity of hyperechogenic pancreas as a marker of GDM via the meta-analytic method.
Methods: Electronic databases such as MEDLINE, EMBASE, Scopus, ClinicalTrials.gov, PROSPERO
International Prospective Register of Systematic Reviews, and Cochrane Central Register of
Controlled Trials were searched from inception of each database. No language restrictions were applied. We then calculated risk ratios for GDM via the meta-analytic method. Data was divided into four groups based on data obtained from case-control studies: +GDM +fetal hyperechogenic pancreas; +GDM -fetal hyperechogenic pancreas; -GDM +fetal hyperechogenic pancreas; -GDM -fetal hyperechogenic pancreas. The software Ref Manager was utilized to perform the Mantel-Haenszel method and Restricted maximum-likelihood estimator for tau^2.
Results: Two studies, with a total of 145 pregnant women and 141 pregnant women, respectively, were analyzed. We determined the risk ratio of GDM and hyperechogenicity to be 3.34 via the random effects model with a p-value of <0.0001 [95% CI, 1.56- 7.17]. We determined the risk ratio to be 3.25 via the common effect model with a p-value of 0.0019 [95% CI, 2.38- 4.44]. To quantify heterogeneity, we obtained values of tau^2 = 0.2482; tau = 0.4982; I^2 = 81.7% [22.7%; 95.7%]; H = 2.34 [1.14; 4.82]. Our test of heterogeneity yielded Q= 5.48 and d.f.= 1 (p=0.0192).
Discussion: We found an association between prenatally detected hyperechogenic fetal pancreas and development of GDM in the mother with a RR of 3.34 [1.56 - 7.17]. We propose the incorporation of fetal pancreas echogenicity detection in the routine detailed fetal ultrasound assessment, potentially helping the clinician in the diagnosis of GDM. We focused our meta-analysis on the association between fetal hyperechogenic pancreas and diagnosis of GDM, but the single identified studies also suggest an association between fetal hyperechogenic pancreas and fetal characteristic and neonatal outcomes. Regarding outcomes of the fetus, the studies showed that fetuses with increased pancreatic hyperechogenicity are more likely to experience increased birth weight], lower APGAR scores, and higher NICU admission rate. Therefore, detection of hyperechogenic fetal pancreas on ultrasound should be implemented as an indicator of GDM. A potential hypothesis of pancreatic hyperechogenicity describes the process of excess maternal glucose crossing the placenta and being stored in the fetus as body fat. This is commonly noted in the shoulders and subcutaneous abdominal tissue of the fetus, which is characterized as macrosomia. Hyperechogenicity in the fetal pancreas may develop by the same mechanism of stored fat. One study confirmed that in adults, fatty hyperechogenic pancreas is not a benign finding and should not be accepted as a normal screening, as it may hint at deleterious underlying consequences.
Conclusion: Overall, our meta-analysis highlights hyperechogenicity of the fetal pancreas as a potential
marker for GDM. Therefore, utilizing hyperechogenicity of the fetal pancreas as a complementary screening tool may be auspicious in the identification and management of pregnant women with GDM. Ultrasound is a relatively quick, cost-efficient exam, and thus this may provide clinicians with a simple way to diagnose and prevent the development of GDM. In addition, changes in the pancreas in the fetal period may affect the pancreatic function into adulthood. Ultimately, our results indicate that there is a need for more research to be done examining the interplay between GDM and fetal hyperechogenic pancreas.
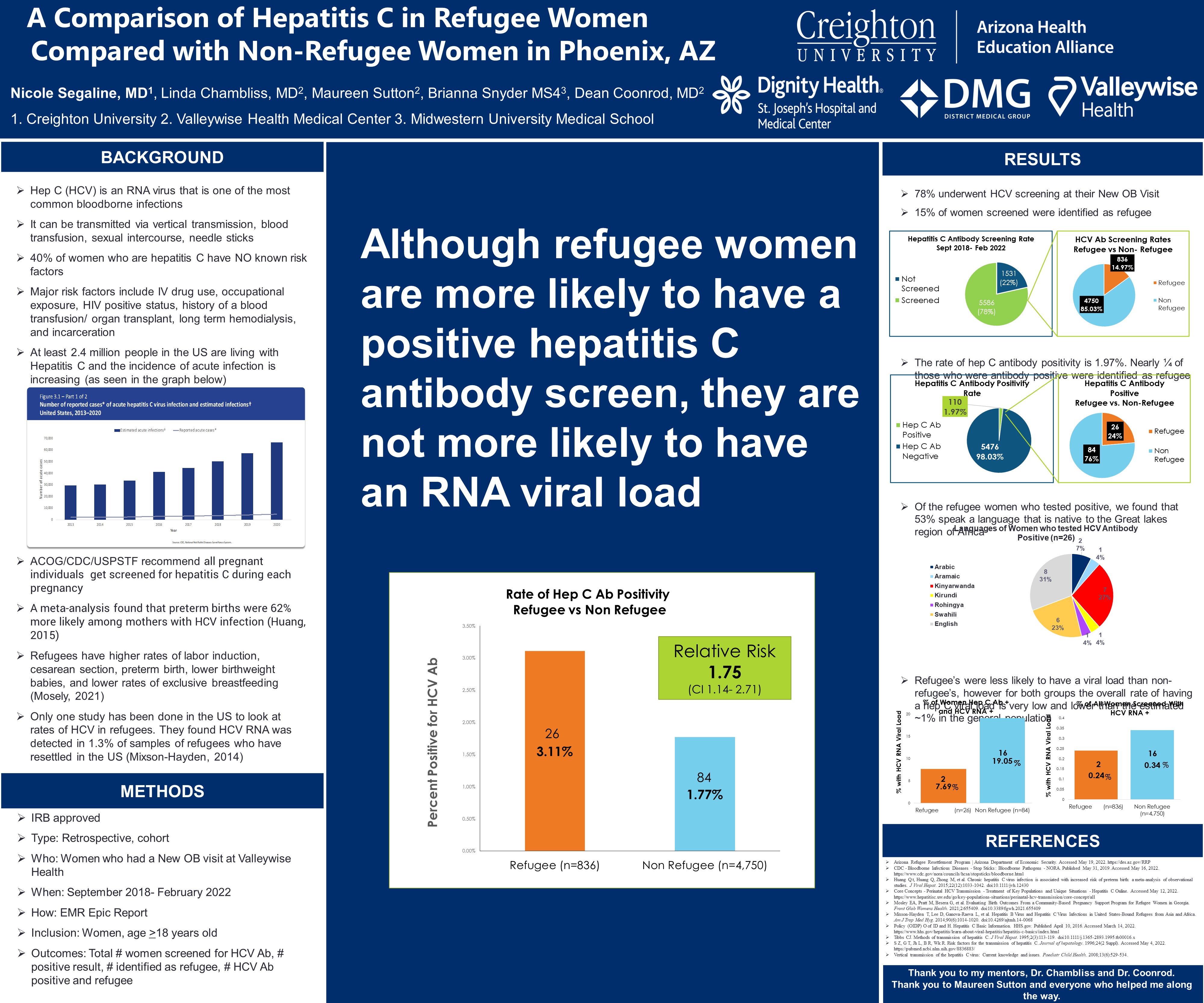
Nicole Segaline MD, Linda Chambliss MD, Maureen Sutton MPH, Brianna Snyder MS4, Dean Coonrod, MD MPH
Introduction: There are extremely limited studies on the rates of Hepatitis C in refugee populations, especially in the United States. Hepatitis C virus (HCV) is one of the most common bloodborne infections and can be associated with significant long term maternal and fetal morbidity. This study aims to compare the number of women who screen positive for hepatitis C antibody at their initial prenatal visit in the refugee population compared to the non-refugee population.
Methods: A retrospective cohort study was conducted with women who had established prenatal care at the only safety net hospital in Phoenix, Arizona between September 2018-February 2022. Following the guidelines of the American College of Obstetricians and Gynecologists (ACOG), our institution completes universal screening for HCV for pregnant women. The electronic medical record system was queried and identified women who had an initial prenatal visit during this time and underwent hepatitis C antibody screening. The report then characterized women by their refugee status. Additional variables acquired included demographic features, risk factors for hepatitis, and co-morbidities. The primary outcome of refugee status and HCV screening result were analyzed using relative risks. Chi-square and t-tests were used to examine relationships of the variables as potential confounders.
Results: During the 3.5-year time period, there were 7,117 initial prenatal visits. Of that, 5,586 women were screened for Hepatitis C, for an overall screening rate of 78%. There were 110 women who had a positive hepatitis C antibody screen, for a total positivity rate of 1.97%. Of the non-refugee women screened 84 out of 4750 (1.77%) had a positive result. There were 836 refugee women screened and 26 had a positive screen, for a positivity rate of 3.21%. The relative risk was 1.75 (95% CI 1.14-2.71). When examined by primary language, refugees who spoke a language native to the Great Lakes region of Africa were the groups most likely to have a positive screen.
Conclusions: These results show that refugee women have a 75% higher rate of testing positive for the hepatitis C antibody than non-refugee women. This analysis supports refugee status as a risk factor for screening positive for hepatitis C antibody. In addition to the barriers refugee women already face including increased risk of preterm birth, labor induction and cesarean section, hepatitis C can not only increase risk for preterm labor but also have long term consequences to the mother and the fetus via vertical transmission. Identifying risk factors can improve care for refugee women in the peripartum and intrapartum periods.
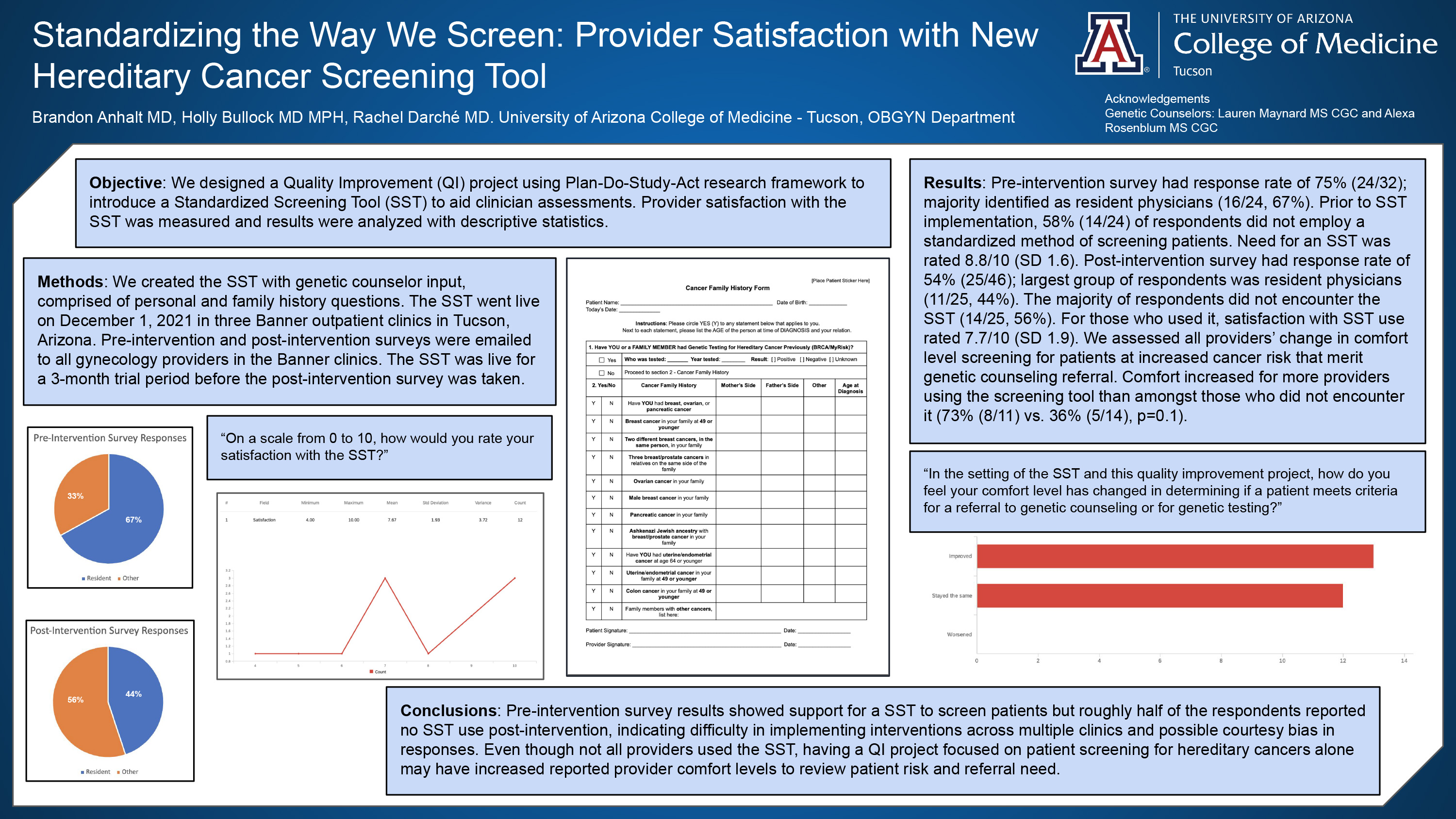
Brandon Anhalt MD, Rachel Darche MD, Holly Bullock MD, MPH
Introduction: The American College of Obstetricians and Gynecologists (ACOG) recommends hereditary cancer risk assessments be performed as routine care to identifying patients and families who may have increased risk of developing certain types of cancer. We designed a Quality Improvement (QI) project using Plan-Do-Study-Act research guidelines to introduce a Standardized Screening Tool (SST) to aid clinician assessments.
Methods: We created the SST with genetic counselor input, comprised of personal and family history questions. SST went live on 12/1/2021 in three Banner outpatient clinics in Tucson, Arizona. Pre-intervention and post-intervention surveys three months later were emailed to all gynecology providers in the Banner clinics. Results were analyzed with descriptive statistics.
Results: Pre-intervention survey had response rate of 75% (24/32); majority identified as resident physicians (16/24, 67%). Prior to SST implementation, 58% (14/24) of respondents did not employ a standardized method of screening patients. Need for an SST was rated 8.8/10 (SD 1.6). Post-intervention survey had response rate of 54% (25/46); majority were resident physicians (11/25, 44%). The majority of respondents did not encounter the SST (14/25, 56%). For those who used it, satisfaction with SST use rated 7.7/10 (SD 1.9). We assessed all providers’ change in comfort level screening for patients at increased cancer risk that merit genetic counseling referral. Comfort increased for more providers using the screening tool than amongst those who did not encounter it (73% (8/11) vs. 36% (5/14), p=0.1).
Conclusion/Implications: Pre-intervention survey results showed support for a SST to screen patients but roughly half of the respondents reported no SST use post-intervention, indicating difficulty in unrolling interventions across multiple clinics and possible courtesy bias in responses. Even though not all providers used the SST, having a QI project focused on patient screening for hereditary cancers alone may have increased reported provider comfort levels to review patient risk and referral need.
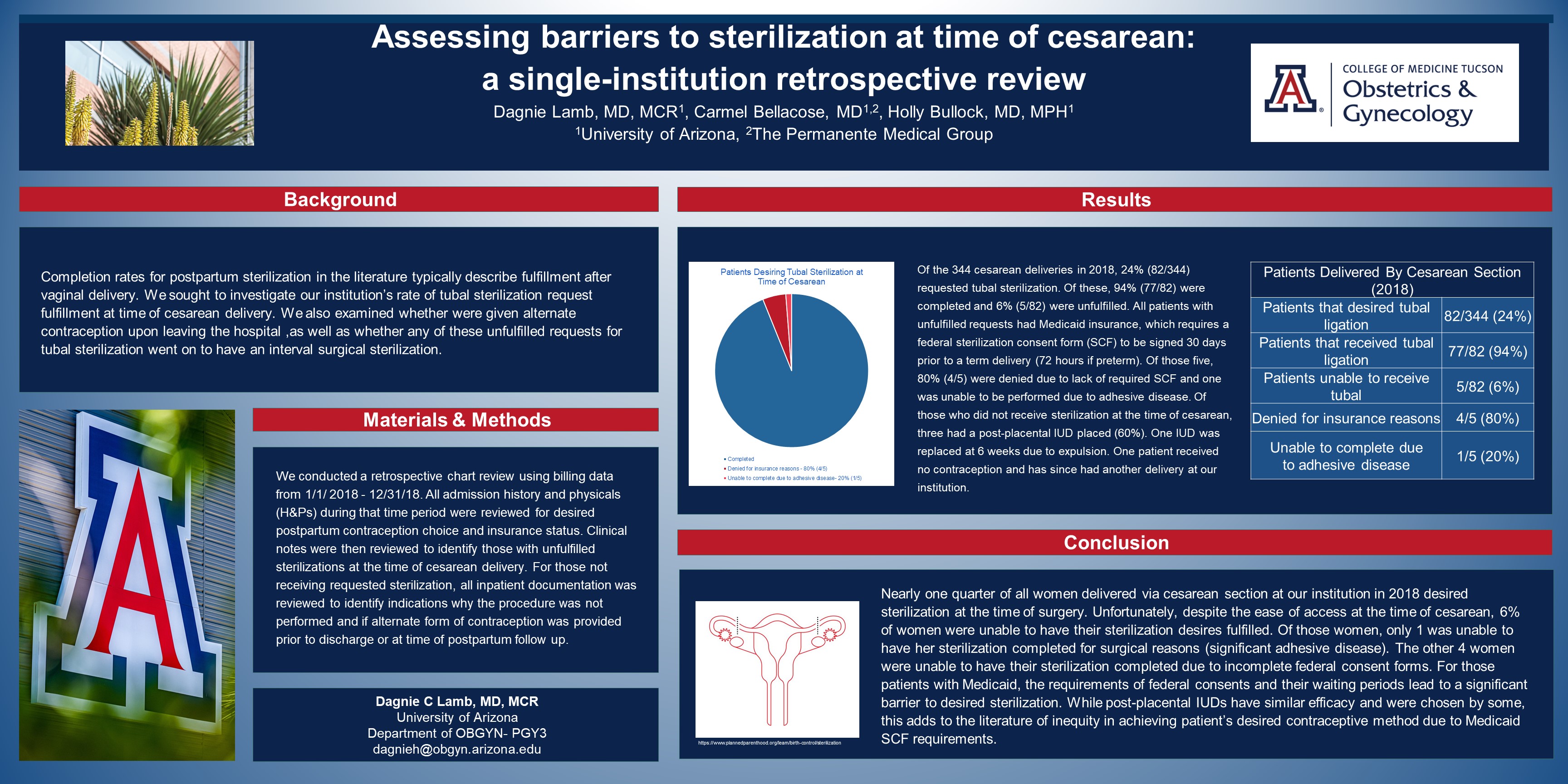
Dagnie Lamb MD, MCR, Carmel Bellacose MD, Holly Bullock MD, MPH
Introduction: Completion rates for postpartum sterilization in the existing literature typically describe fulfillment after vaginal delivery. We sought to investigate our institution’s rate at time of cesarean delivery (CD).
Methods: We conducted a retrospective chart review using billing data from 1/1/ 2018 - 12/31/18. All admission history and physicals (H&Ps) for CDs were reviewed for desired postpartum contraception choice and insurance status. Clinical notes were then reviewed to identify those with unfulfilled sterilizations at the time of CD. For those not receiving requested sterilization, all inpatient documentation was reviewed to identify indications for lack of sterilization fulfillment and if alternate form of contraception was provided prior to discharge or at time of postpartum follow up.
Results: Of the 344 cesarean deliveries in 2018, 24% (82/344) requested tubal sterilization. Of these, 94% (77/82) were completed and 6% (5/82) were unfulfilled. All patients with unfulfilled requests had Medicaid insurance. Of those five, 80% (4/5) were denied due to lack of required federal sterilization consent form (SCF) and one was unable to be performed due to adhesive disease. Of those who did not receive sterilization at the time of CD, three had a post-placental IUD placed (60%). One IUD was replaced at 6 weeks due to expulsion prior to discharge. One patient received no contraception and has since had another delivery at our institution.
Conclusions: Nearly one quarter of all women delivered via CD at our institution in 2018 desired sterilization at the time of surgery. Unfortunately, 6% of women were unable to have their sterilization desires fulfilled predominantly due to lack of federal SCF. While post-placental IUDs have similar efficacy and were chosen by some, this adds to the literature of inequity in achieving patient’s desired contraceptive method due to Medicaid SCF requirements.
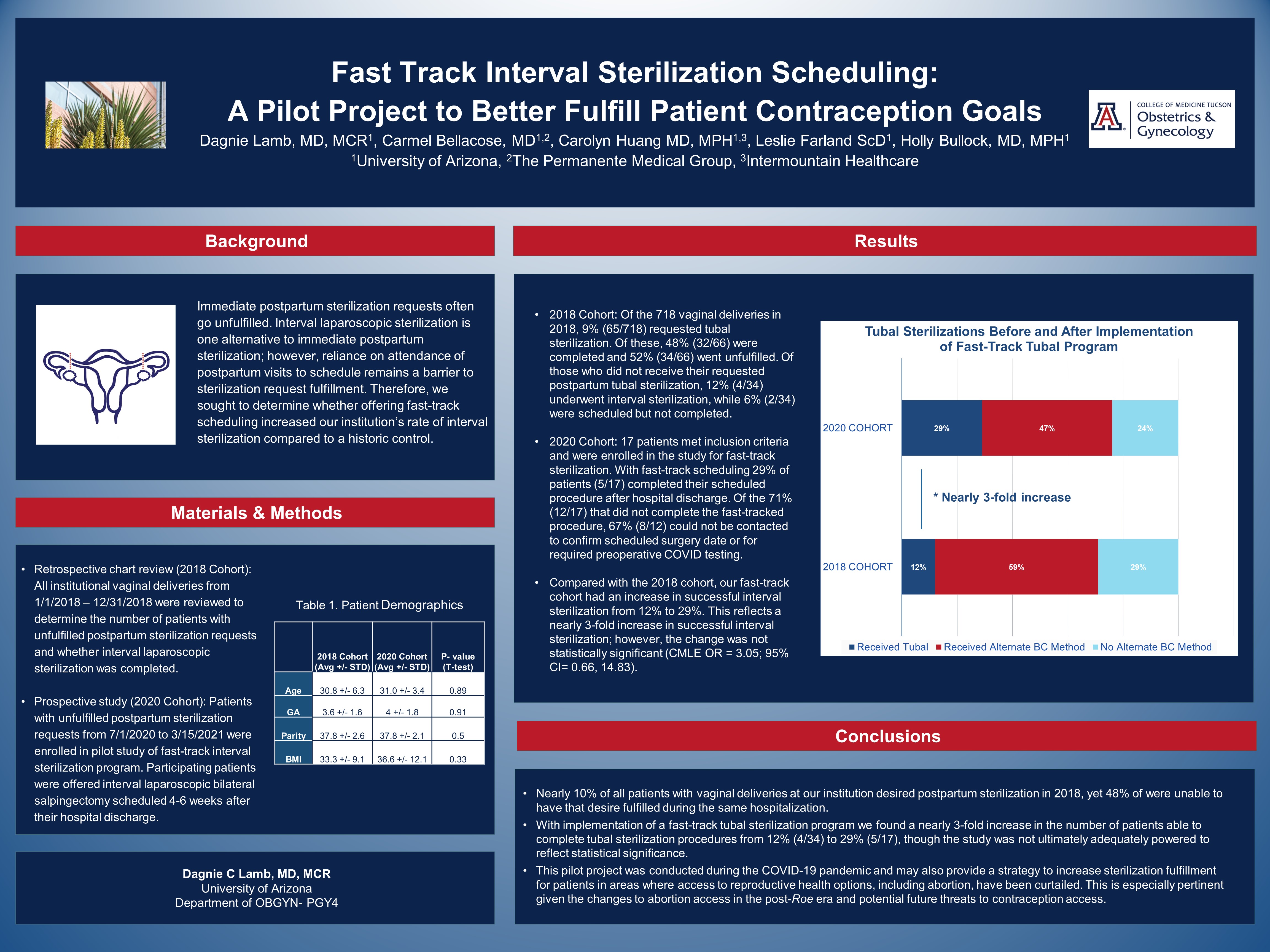
Dagnie Lamb MD, MCR, Carmel Bellacose MD, Carolyn Huang MD MPH, Holly Bullock MD MPH
Introduction: Immediate postpartum sterilization requests often go unfulfilled. Interval laparoscopic sterilization is one alternative to immediate postpartum sterilization; however, reliance on attendance of postpartum visits in order to schedule remains a barrier to sterilization request fulfillment. Therefore, we sought to determine whether offering fast-track scheduling increased our institution’s rate of interval sterilization compared to a historic control.
Methods: We conducted a retrospective chart review of all vaginal deliveries from 1/1/18 – 12/31/18 to determine the number of patients with unfulfilled postpartum sterilization requests and whether interval laparoscopic sterilization was completed. We then implemented a pilot fast-track interval sterilization program enrolling patients with unfulfilled postpartum sterilization requests from 7/1/20 to 3/15/21. Participating patients were offered fast-track interval laparoscopic bilateral salpingectomy scheduled 4-6 weeks after their hospital discharge.
Results: In 2018, 66 of 718 (9%) postpartum patients desired sterilization after vaginal delivery, however, 52% of those requests were unfulfilled with 4 completing interval sterilization procedures (12%). During the pilot period, 17 postpartum patients with unfulfilled postpartum sterilization goals consented to fast-track scheduling, with 29% completing their procedure . This resulted in a 3-fold increase in successful interval sterilization however the change was not statistically significant (CMLE OR = 3.05 95% CI= 0.66, 14.83; ) .
Conclusion: Implementing fast track scheduling did result in an increase in fulfilled contraception goals for patients. This pilot project was conducted during the COVID-19 pandemic and may also provide a strategy to increase sterilization fulfillment for patients in areas where access to reproductive health options, including abortion, have been curtailed.
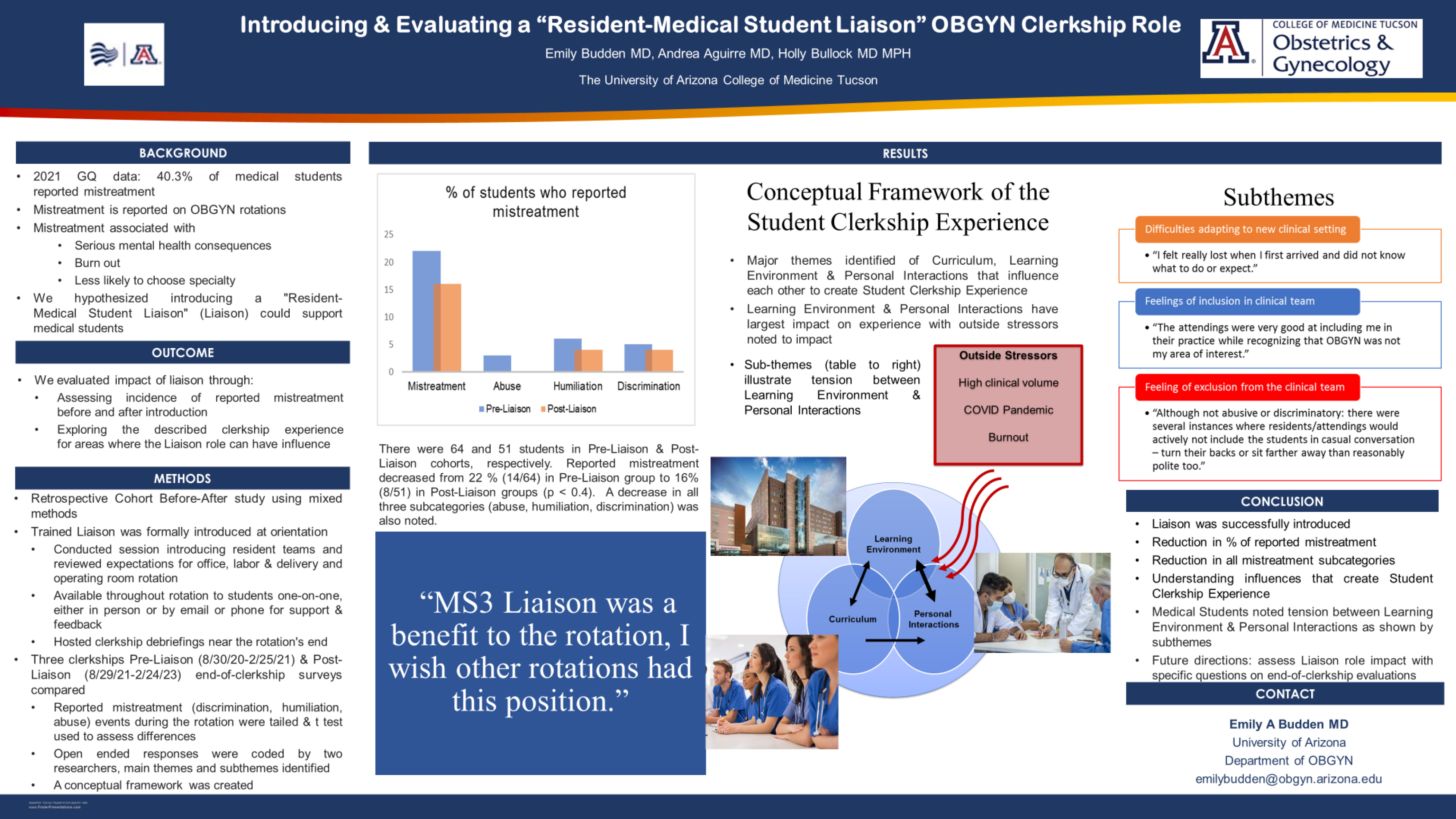
Emily Budden MD, Andrea Aguirre MD, Holly Bullock MD, MPH
Purpose: We sought to create a novel quality improvement (QI) project to better support medical students (MS) during their six week OBGYN clerkship experience.
Background: MS mistreatment is a common reported occurrence on OBGYN rotations. We theorized a “Resident-Medical Student Liaison” (Liaison) could offer individualized support to MS and reduce reported student mistreatment.
Methods: This QI project was a Retrospective Cohort (Before-After Study) using mixed methods. An R3 OBGYN Resident Liaison was trained and introduced to each OBGYN clerkship group at in-person orientation. They reviewed MS expectations for office, labor & delivery and operating room rotation portions. MS could seek out or provide feedback to the Liaison one-on-one, either in person or by email or phone. The Liaison hosted clerkship debriefings near the rotation’s end. Two MS cohorts, each spanning 3 clerkships, were compared before and after the initiation of the Liaison. Pre-Liaison spanned 8/30/21-2/25/22 while post-Liaison spanned (8/29/22-2/24/23). In end-of-clerkship surveys, MS are asked to report experienced mistreatment (discrimination, humiliation, abuse) during the rotation. Descriptive statistics were used to assess for differences between cohorts. Open-ended responses were coded by two researchers, themes and concepts delineated, and data analyzed.
Results: Pre-Liaison included 64 MS versus 51 MS in the Post-Liaison cohort. Percentage of students reporting incidents of mistreatment decreased from 2.2 % (14/64) to 1.6% (8/51) from pre- to post-Liaison groups, p <0.4. Qualitative data yielded themes related to curriculum, learning environment, and personal interactions all influencing the student clerkship experience. Difficulties adapting to new clinical settings and feelings of inclusion/exclusion in the clinical team were subthemes describing the tension between the learning environment and personal interactions.
Conclusions: Following Liaison introduction there was a reduction in the number of students reporting mistreatment, though this was not statistically significant. Qualitative data highlighted the tension that medical students feel navigating new learning environments and the influence that personal interactions on the rotation have on the overall clerkship experience. It is in this area that the Liaison can act as a positive force to offer MS clerkship-specific support.
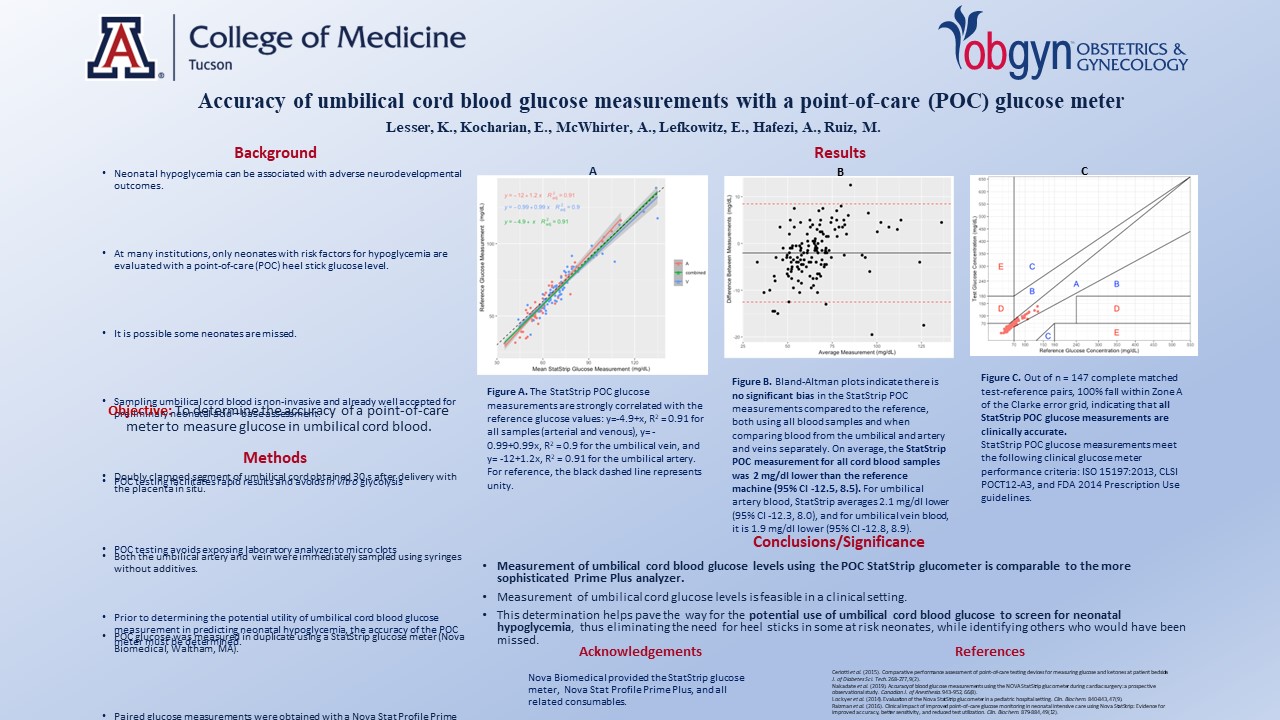
Karen Lesser, Elida Kocharian, Amanda McWhirter, Eli Lefkowitz, Autri Hafezi, Maria Ruiz
Background: Neonatal hypoglycemia can be associated with adverse neurodevelopmental outcomes. At many institutions, only neonates with risk factors for hypoglycemia are evaluated with a point-of-care (POC) heel stick glucose level. Umbilical cord blood is already well accepted for preliminary neonatal acid – base assessment. POC testing of umbilical cord blood facilitates rapid results and avoids glycolysis. Prior to determining the potential utility of umbilical cord blood glucose in predicting neonatal hypoglycemia the accuracy of the point-of-care meter must be determined.
Objective: To determine the accuracy of a POC meter to measure glucose in umbilical cord blood.
Methods: Women undergoing scheduled cesarean deliveries at term, who were not in labor, were consented for participation in this study. A doubly clamped segment of umbilical cord was obtained 30 s after delivery with the placenta in situ. Both the umbilical artery and umbilical vein were immediately sampled using syringes without additives. POC glucose was measured in duplicate using a StatStrip glucose meter (Nova Biomedical, Waltham, MA). A clot catcher was attached to the syringe to measure a paired sample with a Nova Stat Profile Prime Plus (Nova Biomedical, Waltham, MA) tabletop analyzer, our reference for glucose measurement. This was chosen, rather than the hospital lab analyzer, secondary to concerns regarding microclots within umbilical cord blood damaging the laboratory machine, as well as avoiding glucose metabolism within the sample by promptly measuring glucose with the reference machine in the same location. Linear regression analysis was performed to assess the relationship between glucose measurements from the StatStrip POC meter and the Prime Plus analyzer. Bland-Altman plots were generated to evaluate bias between the POC and reference analyzer glucose measurements.
Results: The StatStrip POC glucose measurements were strongly correlated with the reference glucose values: y=-4.9+x, R2 = 0.91 for all samples (arterial and venous), y=-0.99+0.99x, R2 = 0.9 for the umbilical vein, and y= -12+1.2x, R2 = 0.91 for the umbilical artery. Bland-Altman plots indicate there is no significant bias in the StatStrip measurements compared to the reference, both using all blood samples and when comparing blood from the umbilical artery and vein separately. On average, the StatStrip POC measurement for all cord blood samples was 2 mg/dl lower than the reference machine (95% CI -12.5, 8.5). For umbilical artery blood, StatStrip averages 2.1 mg/dl lower (95% CI -12.3, 8.0), and for umbilical vein blood, it is 1.9 mg/dl lower (95% CI -12.8, 8.9).
Conclusion: Measurement of umbilical cord blood glucose levels using the POC StatStrip glucometer is feasible and comparable to the more sophisticated Prime Plus analyzer. This determination will help pave the way for the potential use of umbilical cord glucose to screen for neonatal hypoglycemia, thus eliminating the need for heel sticks in some at risk neonates, while identifying others who would have been missed.
Join now & support your local OB/GYN community!
Membership in the Phoenix Ob/Gyn Society is open to all providers specializing in the OB/GYN field including Physicians, Nurse Practitioners and Physician Assistants. Your membership entitles you to our 7 dinner meetings (including dinner for a guest or spouse at our Spring Social Meeting).
Click here to learn more »Meetings are on the 3rd Wednesday of the month at Mastro's City Hall Steakhouse. Dinner meeting topics include a wide variety of subjects of interest to our specialty.
Interested in supporting our annual Resident Research Night, sponsoring a Society dinner meeting, or advertising with us?
Learn more about sponsorship opportunities »Home Become a Member Events RSVP Sponsors Become a Sponsor Dues Job Board Contact
© 2026 Phoenix Obstetrical & Gynecological Society. Phoenix, AZ